By Dr. Belinda Gregory-Head, DDS – Dental Implant Partners, San Francisco
As a practicing dentist with years of experience helping patients transition to and maintain dentures, I know firsthand that the health of your prosthesis directly impacts your oral function, comfort, and long-term oral health. Proper care is not merely about aesthetics. It is about preserving the integrity of the prosthesis, protecting the surrounding oral tissues, and preventing systemic health complications that may arise from poor hygiene. This guide is designed to help you understand denture care at a deeper, clinical level, giving you the tools to extend the lifespan of your dentures while keeping your mouth healthy.
Understanding the Importance of Denture Care
Denture maintenance goes far beyond appearance. When a prosthesis is not adequately cleaned, biofilm composed of bacteria and fungi begins to colonize its surface. Over time, this can lead to infections such as denture stomatitis, angular cheilitis, or exacerbation of periodontal disease in patients with partial dentures. These complications can compromise both oral and systemic health, particularly in medically compromised patients or those with weakened immune systems.
Another reason for meticulous denture care is the direct impact on comfort and function. A clean, well-maintained prosthesis will sit more comfortably against the mucosal tissues and will be less prone to causing irritation, ulcers, or pressure points. Once irritation begins, the cycle of inflammation often perpetuates itself, leading to significant discomfort that could have been avoided with proper preventive care.
Finally, proper care extends the longevity of the prosthesis itself. Acrylic resin, porcelain, and modern composite materials are durable, but they are not impervious to damage. Residual debris and plaque acids can cause surface deterioration, staining, and even micro-fractures over time. As dentists, we design dentures to last, but without consistent maintenance, their functional lifespan can be significantly shortened.
Daily Cleaning Practices
The foundation of denture care is a daily cleaning routine. I always advise my patients that dentures should be removed and cleaned after every meal when possible, or at least twice daily. Simply rinsing them under water is insufficient, as water does not disrupt plaque biofilm. Instead, patients should use a soft-bristled denture brush and a non-abrasive cleanser specifically formulated for prosthetic appliances. Regular toothpaste is not recommended, as its abrasives can microscopically scratch the acrylic, creating niches for bacterial growth.
Equally important is the cleaning of the underlying mucosal tissues. Patients often overlook the necessity of gently brushing the tongue, palate, and alveolar ridges where dentures sit. This prevents fungal overgrowth and promotes healthier tissue resilience, reducing the risk of stomatitis. For partial denture wearers, special attention must be paid to natural teeth, as plaque accumulation around clasps can accelerate caries and periodontal breakdown.
I also encourage patients to establish a consistent nighttime cleaning ritual. Dentures should be removed before sleep to give the oral tissues a chance to recover from mechanical stress. Soaking the prosthesis overnight in an appropriate denture solution not only keeps it clean but also maintains its hydration. Dry acrylic is more brittle and prone to warping, so overnight immersion is as much about preserving the denture as it is about hygiene.
Proper Handling and Storage
Handling dentures requires the same care as handling fragile dental ceramics. Dropping them on a hard surface can cause fractures or tooth dislodgment, so I recommend cleaning them over a folded towel or basin filled with water. This simple precaution significantly reduces the risk of accidental breakage. Furthermore, always use both hands when removing or inserting dentures to avoid bending clasps or stressing one part of the framework.
Storage is equally important for long-term durability. Dentures should never be left to dry out, as desiccation leads to warping and material degradation. When not in use, they should be stored in water or an approved soaking solution. Patients with implant-supported overdentures must be particularly careful, as attachment housings and O-rings can become compromised if exposed to inappropriate chemicals or if left dry for prolonged periods.
I also stress the importance of avoiding hot or boiling water during cleaning or storage. Excessive heat alters the dimensional stability of the acrylic base, leading to ill-fitting dentures that can cause tissue trauma. Once a prosthesis loses its fit due to improper care, relining or remaking may become necessary, which could have been prevented with correct handling habits.
Choosing the Right Cleaning Solutions
The selection of cleaning agents should never be an afterthought. Over-the-counter denture cleansers are generally effective, but patients must be cautious about product selection. Effervescent tablets, for example, are excellent for breaking down biofilm, but prolonged soaking in highly alkaline solutions may affect the longevity of metal clasps on partial dentures. For patients with sensitive mucosa, I sometimes recommend hypoallergenic, alcohol-free formulations to minimize tissue irritation.
Chlorhexidine rinses can play a role in managing recurrent stomatitis, but they must be used judiciously. While effective against fungal and bacterial colonization, overuse can stain prosthetic surfaces and alter taste perception. I typically recommend alternating between chlorhexidine and milder cleansing agents to balance efficacy and safety. Patients with implant overdentures should avoid alcohol-based cleansers altogether, as they can degrade attachment components.
Enzymatic cleansers are another useful adjunct, especially for breaking down organic deposits. They are particularly beneficial for patients with reduced dexterity who may not be able to mechanically clean their dentures as thoroughly. In clinical practice, I tailor recommendations based on each patient’s oral condition, prosthesis material, and systemic health profile.
Preventing and Managing Stains
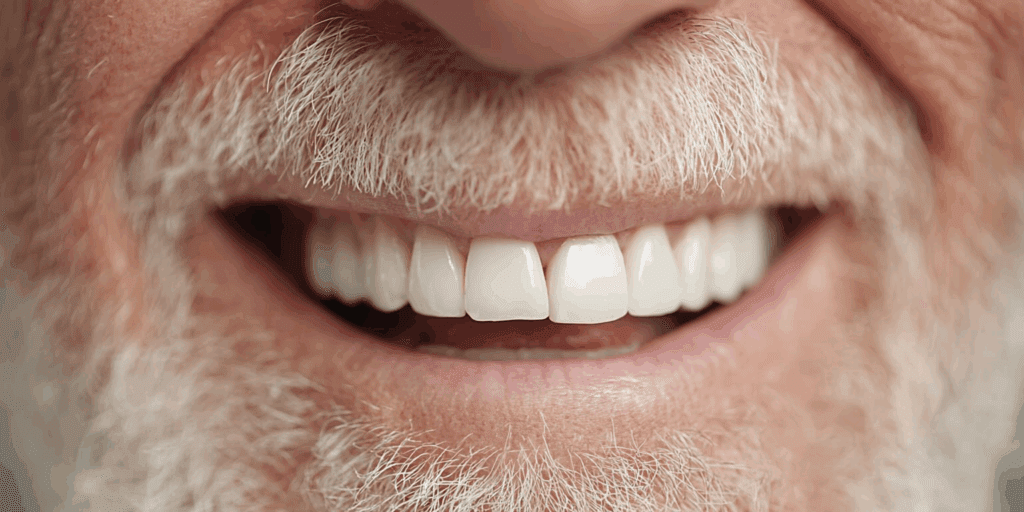
Denture staining is one of the most common concerns patients bring up, and its prevention requires both proper cleaning and dietary awareness. Beverages such as coffee, tea, and red wine, as well as habits like tobacco use, can rapidly discolor acrylic or porcelain surfaces. Once pigments penetrate the micro-pores of the prosthesis, they are challenging to remove without professional intervention. I encourage patients to rinse immediately after consuming staining agents to reduce their impact.
Beyond dietary considerations, the texture of the denture surface plays a major role in stain adherence. Over time, microscopic scratches caused by abrasive brushing or harsh toothpaste can act as retention sites for pigments. This is why I stress the use of soft brushes and non-abrasive cleansers. Patients who are vigilant about surface integrity tend to report fewer cosmetic concerns over the years.
When stains do develop, professional cleaning in a dental office is the safest and most effective method. Ultrasonic cleaning units can remove stubborn deposits without damaging the prosthesis. I advise against do-it-yourself whitening remedies, as many of these, such as household bleach or abrasive powders, can irreversibly damage the denture and cause tissue burns if not thoroughly rinsed.

The Role of Regular Dental Check-Ups
Even with meticulous home care, regular professional evaluations are essential. A prosthesis is not static; the oral tissues and supporting bone beneath it change over time due to resorption and functional forces. What fits well today may become loose or unstable within a few years. During check-ups, I assess not only the prosthesis but also the health of the oral mucosa, tongue, and any remaining natural teeth.
Another reason routine visits are crucial is the early detection of pathology. Ill-fitting dentures can mask or mimic early signs of oral cancer, particularly on the palate and floor of the mouth. By performing thorough intraoral examinations, I can detect subtle lesions or suspicious changes long before they become symptomatic. This is especially important in older adults, who are at increased risk of oral malignancies.
Finally, regular maintenance appointments allow us to professionally clean the prosthesis and adjust its fit. Small relines, adjustments to pressure points, or replacement of worn attachments in implant overdentures can dramatically improve comfort and function. Patients who commit to these visits typically enjoy longer-lasting, healthier outcomes than those who only seek help when problems arise.
Relining, Rebasing, and Replacement
No denture lasts forever, and part of long-term care involves recognizing when modifications or replacements are needed. Relining involves resurfacing the tissue side of the denture to improve its fit as the alveolar ridge resorbs. This is often required every few years, depending on the rate of bone remodeling. Patients sometimes mistake the need for relining as a sign their denture is “worn out,” when in reality the base material and teeth may still be structurally sound.
Rebasing, on the other hand, is a more extensive procedure where the entire acrylic base is replaced while keeping the prosthetic teeth. This may be necessary when the base is significantly worn or stained but the teeth remain serviceable. It is a cost-effective alternative to a full replacement, though not always appropriate depending on the degree of wear.
Eventually, however, replacement becomes inevitable. Acrylic teeth wear down, vertical dimension collapses, and esthetics are compromised. In my experience, most complete dentures require replacement approximately every 7–10 years, though this varies widely depending on patient habits, oral anatomy, and maintenance. Timely replacement ensures that patients maintain functional efficiency and a youthful, balanced facial profile.
Caring for Partial Dentures
Partial dentures present unique challenges compared to complete dentures. Because they rely on natural teeth for support and retention, oral hygiene must be even more rigorous. Plaque tends to accumulate around metal clasps, increasing the risk of root caries and periodontal compromise in abutment teeth. I emphasize targeted brushing and the use of adjunctive aids such as interdental brushes or water flossers for these critical sites.
Partial dentures also create mechanical forces that must be monitored over time. If the supporting teeth or tissues change, the distribution of stress may cause mobility or even tooth loss. This is why regular adjustments and occlusal evaluations are indispensable. A well-fitting partial can serve as a stable, long-term solution, but a neglected one can accelerate tooth loss and lead to more complex restorative needs.
Additionally, patients with partial dentures often underestimate the need for periodic replacement. As remaining teeth shift or are lost, the partial must be modified or remade to preserve harmony in occlusion. Ignoring these changes risks destabilizing the arch, which may eventually require transitioning to a complete denture or implant-supported prosthesis.
Implant-Supported Dentures: Special Considerations
Implant-supported overdentures are increasingly popular due to their superior stability and function. However, their care requirements differ from traditional dentures. Attachments such as locator abutments or bars must be meticulously cleaned to prevent peri-implant disease. Failure to remove biofilm from these sites can lead to mucositis or peri-implantitis, both of which jeopardize the longevity of the implants themselves.
Patients with implant overdentures must also be aware of component wear. O-rings, nylon inserts, and clips lose their retentive strength over time and must be replaced periodically. I counsel my patients that this is a normal maintenance requirement, not a failure of the system. Regular follow-up visits allow us to monitor wear and replace components proactively, maintaining optimal stability and function.
Another key factor is occlusal management. Implant overdentures distribute forces differently than tissue-supported dentures, and improper occlusion can lead to accelerated wear of the prosthetic teeth or stress on the implants. Periodic professional evaluation ensures that occlusal forces remain balanced, protecting both the prosthesis and the underlying implant structures.
Nutrition and Lifestyle Factors
The foods you eat and the habits you maintain play a pivotal role in denture longevity. Hard, sticky, or overly tough foods can place undue stress on prosthetic teeth and bases, leading to fractures or wear. Patients transitioning to dentures often need guidance on food selection, at least initially, to avoid mechanical complications. Over time, most patients adapt, but a mindful diet continues to protect both prosthesis and oral tissues.
Lifestyle choices such as smoking and alcohol consumption further complicate denture care. Tobacco accelerates staining, increases the risk of stomatitis, and compromises healing in the event of tissue trauma. Alcohol can dry oral tissues, exacerbating irritation and reducing resilience to mechanical stress. As with natural dentition, dentures perform best in a healthy oral environment, free from the inflammatory burden of these habits.
Hydration also deserves mention. Adequate salivary flow is critical for denture comfort, as saliva acts as a natural lubricant and antimicrobial agent. Patients with xerostomia, often caused by medications or systemic conditions, require tailored management strategies such as saliva substitutes or prescription sialogogues. These interventions not only improve comfort but also reduce microbial colonization and tissue trauma.
Extending the Lifespan of Your Dentures
Ultimately, denture longevity is the result of a partnership between patient and dentist. From the patient’s perspective, consistent hygiene, careful handling, and mindful lifestyle choices provide the foundation. From the clinician’s perspective, ongoing evaluation, adjustments, and timely intervention preserve both prosthesis and oral tissues. This dual commitment ensures the prosthesis functions optimally for as long as possible.
I remind my patients that dentures are not passive devices. They interact constantly with the dynamic oral environment. Bone resorption, mucosal changes, and occlusal wear are inevitable, but their impact can be minimized through proactive care. Patients who approach denture care as an integral part of their health routine invariably experience better outcomes than those who view it as an afterthought.
By integrating professional guidance with daily diligence, dentures can remain comfortable, functional, and esthetically pleasing for many years. For patients in San Francisco and beyond, my message is always the same: caring for your dentures is caring for your overall health. A well-maintained prosthesis does more than restore a smile. It restores quality of life.
About Dental Implant Partners
At Dental Implant Partners, I have had the privilege of serving patients in San Francisco for over 25 years, focusing on restoring smiles with precision and care. Our practice is built on a foundation of expertise in prosthetic dentistry, with a team of prosthodontists, general dentists, and hygienists who bring extensive training and genuine dedication to each patient’s needs. Because our hygienists were trained as dentists, they provide an exceptional level of clinical insight that ensures our patients receive the highest quality care possible.
We offer a comprehensive range of restorative treatments, from simple fillings to advanced dental rehabilitations involving implants. While we are known for our expertise in implant dentistry, we are equally committed to helping patients who rely on dentures, particularly those for whom implants are not the right solution. Crafting and maintaining well-fitting dentures is an art that requires both technical skill and an understanding of the unique challenges each patient faces, and it is a service we take pride in providing.
Our practice is not only about delivering clinical excellence but also about building long-term relationships. Patients trust us because we approach their care with integrity, compassion, and attention to detail, all within a beautiful suite overlooking the San Francisco Bay. If you are seeking expert guidance in dentures, implants, or any form of restorative dentistry, we would love to welcome you to our practice. Contact us today to schedule a consultation and take the next step toward a healthier, more confident smile.